Comparing the cost-utility of HPV vaccination strategies in the United Kingdom Case Study Solution
Methods
We undertook a cost-utility analysis to compare the costs and outcomes of HPV vaccination for equivalent and 9-valent vaccines. To measure outcome, we used quality-adjusted life years (QALYs); with National Institute for Health and Care Excellence (NICE) considering interventions costing the NHS less than £20,000 per QALY gained as cost effective. All outcomes and costs after their first year were discounted at an annual rate of %
Model structure
Two treatment options were considered: the quadrivalent vaccine versus the 9-valent vaccine. The analysis was taken from a UK National Health Service (NHS) perspective, with costs calculated in 2021 UK pound. The time horizon for the treatment of patients with the two HPV vaccines was 70 years, reflecting the average life expectancy of patients treated with the two HPV vaccines. A discount rate of % was applied to all costs and benefits.
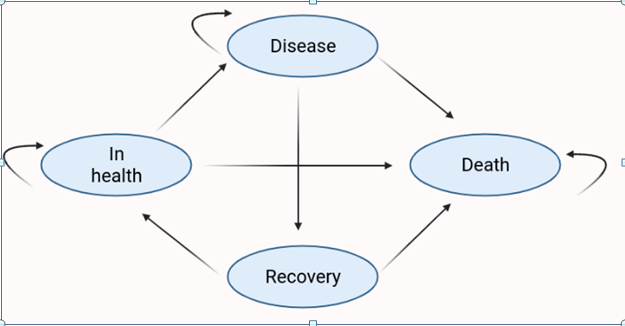
We have produced a Markov model, which simply demonstrates the concept that future states are independent of past states, and that with each step, the model may transition between states, accompanied by a given probability. Whilst hypothetically there are eight human papilloma virus-related health states, for ease of calculation, we have reduced this to four (Ock et al., 2016). Our outcomes were expressed in QALYs. Costs for sick individuals in both control and intervention have been adjusted from 2015 figures at a rate of 1.5% (Curtis and Burns, 2015).
https://hqlo.biomedcentral.com/articles/10.1186/s12955-016-0566-8 the eight states are found in this paper
Figure 1: Simple Markov Model to portray the variation of stages for CC
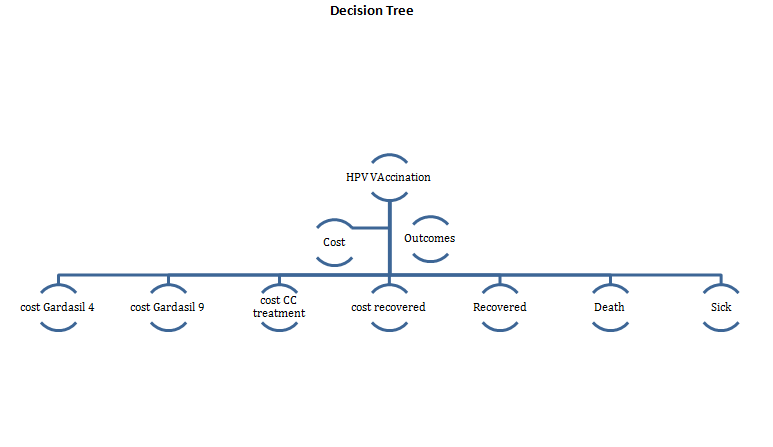
Management strategies
In terms of treatment options we selected two models comparing the G4 against the G9 vaccine. In this case we assumed that each of our interventions required two doses of each vaccine, with costs inflated for this as required. In the UK, there is a routine HPV immunization programme for schoolgirls and boys aged 12-13 years.1 The national NHS HPV vaccination programme currently uses the Gardasil 4 vaccine only.1
In this model, we assume the following:
- girls and boys under age 14 years were not sexually active.
- The vaccinated girls and boys would receive a full vaccination series of 2 doses before they reach the age of 15 years
- The vaccine will be used in combination with existing HPV screening and treatment procedures
The reference vaccination strategy was defined to be routine HPV vaccination of girls and boys between ages 9 and 14 years.
In the analysis, individuals were given the respective vaccines at the beginning of the simulation. The following health states were established based on the natural history of HPV infection:
- Well: healthy
- Sick: HPV infected, genital warts, mild cervical intraepithelial neoplasia (CIN 1), moderate cervical intraepithelial neoplasia (CIN 2), severe cervical intraepithelial neoplasia or carcinoma in situ (CIN 3), invasive cervical cancer (ICC) (stages I-IV)
- Dead: death from cervical cancer.
Since different proportions of oropharyngeal, anal, penile, and vulvar cancers are caused by HPV, and it is difficult to measure the impact of vaccination on the incidence of HPV caused by the strains covered, these cancers were not included in the model.
On the basis of trials showing high efficacy of prophylactic HPV vaccines against persistent infection and vaccine type–specific CIN grades 2 and 3, vaccination efficacy was assumed to be 100 percent.2,3 The cost of vaccination was set at ?? per series, and the duration of vaccine protection was believed to be lifelong.
Probabilities? - assumptions
Costs
To calculate the price of both treatment options, a micro-costing approach was used to calculate the cost of the two treatment option pathways. The cost of medical therapy for the sick was estimated to be ….
Tracey H Sach, e. a. (2016). Applying micro-costing methods to estimate the costs of pharmacy interventions: an illustration using multi-professional clinical medication reviews in care homes for older people.
Costs were obtained from the literature, crucially from the …………. For the vaccines, official list prices per dose for 9-valent and quadrivalent vaccines were used: £ ……..quadrivalent and £ …..for the 9-valent. In the UK, routine HPV vaccination with two doses is the current recommendation for females aged 9-14 years. However, three doses is necessary for the vaccination of girls aged 15-17 years. A further breakdown of the costs and interventions can be found in Table 1.
Table 1: Costing of interventions and vaccines
| Variable | Cost | Reference |
| G4 | ||
| G9 | ||
| Administration charge | ||
| CC medical therapy |
Outcomes
……..
Probabilities
……
Table 2: Transition probabilities for our Markov Model
| Movement from | To | Range | Source | ||
| G4 | Well | Well | 0.9940 | 0-1 | Association of British Pharmaceutical Industry., 2021 |
| Well | Sick | 0.0045 | 0-1 | ||
| Well | Dead | 0.0015 | 0-1 | ||
| Sick | Well | 0.000 | 0-1 | ||
| Sick | Sick | 0.996 | 0-1 | ||
| Sick | Dead | 0.0035 | 0-1 | ||
| G9 | Well | Well | 0.999 | 0-1 | |
| Well | Sick | 0.00075 | 0-1 | ||
| Well | Dead | 0.00025 | 0-1 | ||
| Sick | Well | 0.000 | 0-1 | ||
| Sick | Sick | 0.9965 | 0-1 | ||
| Sick | Dead | 0.0035 | 0-1 |
Table X: Utility scores for our Markov Model
| Utilities | Base-Case Value | Univariate sens. Analysis | Range | Source |
| Well | 1 | Ock et al., 2016 | ||
| Sick | 0.71 | |||
| Dead | 0 | 0 |
Measuring cost-effectiveness
Cost-effectiveness of the G9 vaccine compared to the G4 vaccine was compared in terms of the incremental cost per QALY gained, or ICER. The ICER was calculated by dividing the cost (£) by the outcome effect (QALYs). The lower and upper limit of the maximum willingness to pay for a QALY in the UK is from £20,000 to £30,000.
Sensitivity analysis
The sensitivity analysis has been carried out by using a minimum and a maximum discount rate in order to find out the discounted costs for the Gardasil 4 and 9, the cost for CC treatment and the recovery cost. The minimum discount rate is calculated as 0.126297 and the maximum discount rate is calculated as 0.96618.
……Results
The ICER of G9 compared to G4 was …..
Assuming a cohort of 100000 patients, over a 70 year cycle,
Table 3;
| Variable | G9 | G4 |
| Discounted cost (£) | At Min = 29603232.214
At Max = 22646678.27 |
At min = 2797369.213
At max = 21400068.84 |
| Difference in discounted cost (£) | At Min = 162954.0008
At Max = 1246609.428 |
|
......................
Comparing the cost-utility of HPV vaccination strategies in the United Kingdom Case Study Solution
This is just a sample partial case solution. Please place the order on the website to order your own originally done case solution.