“Massachusetts General Hospital’s Pre-Admission Testing Area (Pata) Harvard Case” Solution
Introduction
Massachusetts general hospital was found in the year 1811, Boston. It is one of the largest and the most notable healthcare sector in the United States. The association has roughly 23000 representative base having 907 limit of bed for patients. Due to its extraordinary services, people from all over the country travel to get treatment from the hospital.(McCarty,2012)The perioperative clinical division of the hospital principally incorporates pre-operative, intra-operative and post-operative care and recovery. Despite of its most notable performance among its competitors, the achievements were confined by the issues made by PATA (Pre-admission testing area).
Pre-Admission Testing Area (PATA)
PATA stands for Pre-Admission Testing Area. The mission of the PATA was quiet basic. It was conducted to pre-decide that how a particular patient will respond to sedatives during operation. The reason behind the PATA was to understand the patient ability to go through the issuance of tranquilizers. The report then sent to the doctor for postoperative care. However, it has been seen that the beginning of PATA gave the various issues and difficulties for the facility and association. These issues includes longer waiting time of the patient, OR difficulties and mismanagement of attendants.
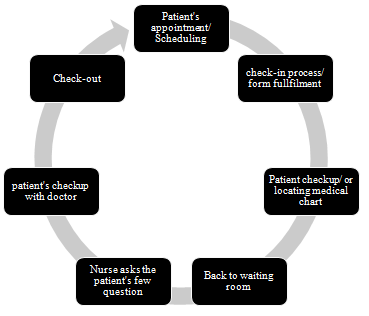
PATA patient flow process
Problem statement
The case highlights the following problem statements;
- The longer waiting time of patient’s
- The capacity was quiet low i.e. only 65 percent of total outpatient’s procedure
- Incomplete checkup of patient’s i.e. long waiting hours frustrated the patient’s and led them to leave the clinic. This results in the delay of postoperative care
- Insufficient working flow and mismanagement
Problem and data analysis
The system of PATA is not adequate and comprises of numerous issues. The primary issue of the PATA is the long waiting time of patient for one visit. It has been seen that the normal holding up time of the patient is around 4 hours which was quiet disastrous and makes the patient despondent. The PATA was planned to run from 8 am to 5 pm, but because of long holding up hours, the time has stretched out to 8pm. This has made the overutilization of staff and medical caretakers which ultimately increases the error rate.
Moreover, the variability of the service rate is unpredictable. It has been seen that most of the time individuals have leftthe clinic earlyamidst of their appointments because they are fatigued of delaying. Several time individuals periodically made an appearance for activity with incomplete PATA records. This has delayed the evaluation of the doctors because they have been waiting to receive the PATA reports to start their procedure. This results in fluctuations of income rate and productivity loss. This loss has been shown up around 57000 minute’s productivity loss annually. (Kamil, 2011)
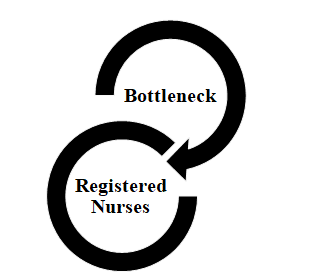
Bottleneck
The case features that the bottleneck is enrolledin RN and MD.In the RN visits, the attendant conducts the patient assessment by asking their clinical history, family foundation, psychological well-being, social government assistance and others. The enrolled medical caretaker would additionally survey which would take around total of 27 minutes for each individual. Moreover, when it comes to MD, it has been seen that the same procedure was followed by the doctor along with the physical assessment. This has increased the long working hours and delayed the patient's care. The RN interaction should be eliminated in order to improve the capacity and pre-admission testing area. The whole course of leading the evaluation of the patient, for example, acquiring data of patient's clinical history, family ancestry, social government assistance, allergies and others ought to be taken care of by the MD.
Alternative options
The chief anesthesia in the MGH, Dr. Jeanine Wiener-Kronish had been given a task to improve and develop the PATA by limiting the time span of the patients. In June, 2009, she proposed a team to work on the task. The group comprised of nursing chief, operating room chief, clinical chief, and a MBA understudies. In the wake of examining the cycle and time span, the team proposed the few alternative options and ideas to improve the PATA. These ideas includes;
- Lessening the volume of the patients
- Expanding the capacity of rooms
- Adding additional time between the appointed times
- Appoints more doctors
Key decision criteria
The decision criteria could be selected on the basis of the bottleneck analysis. It has been seen that the general defect in the PATA technique is that the people have been known to leave in the midst of their appointments since they are exhausted of the long waiting lines. A few time people occasionally showed up for checkup with deficient PATA records. This has postponed the assessment of the specialists since they have been holding back to get the PATA reports to begin their assessment. So, the most important issue that has been seen is the management of the appointments and team. Therefore, the key decision criteria of the issues were assessed on the basis of bottleneck analysis and variability in PATA due to management issues. (see appendix 1)
Alternative analysis
Lessening the volume of the patients
The first alternative option proposed by the team is to lessen the patient's volume i.e. to reduce the volume of the patient per day which ultimately decreases the period of PATA. After analyzing the option, the director replied the capacity of the patient volume in the hospital is already low that is approximately to 65 percent. So, the more reduction in capacity would further lessen the revenue.
Expanding the room capacity
Another alternative option suggests by the team was to expand the room capacity of the patient. This option might be feasible because the MGH has enough capacity of creating more room spaces. It has been that there are few extra rooms available that has been used as a waiting area and have no use. However, if the MGH creates the more room, so it must needs more doctors in order to avoid the shortage of physicians.
Adding additional time between appointments
Another option that suggested was adding additional time between the appointments as it would assist with decreasing the time span of the patients spent in the waiting area. However, this is not the appropriate arrangement as there were patients who had been sitting queue for the RN visits since long. Hence it would not work on the proficiency of the PATA or work on its general interaction.
Appoint more doctors
Another suggested option was to appoint more physicians. It has been seen that the currently hospital contains the 13 physicians in which eight were in RN and remaining five were in MDs. So, appointing more physicians would be the great option for PATA. Moreover, it was noticed that the RN was the bottleneck of the cycles, not the doctors. Adding more doctors would probably make greater intricacy to the activities, for example, on the off chance that more RN are enrolled, the patient would have longer lines with the MD visits.
Recommendations
After analyzing the whole situation and bottle neck of the process, it has been recommended to the Massachusetts General Hospital that;
Long-term recommendations
It is recommended to the MGH that in order to reduce the issue, the best strategy is to improve the process flow on the RN and MD visits. It has been seen that the RN and MD led a similar interaction which is directing evaluations of the patients regarding their health, mental condition, background of the family and allergies. So, the first important recommendation for the team is that they could take individual data through telephone, email, and site before their appearance to the emergency clinic. This will save the time of the patient. Moreover, it is also recommended to MGH to appoint more nurses in order to reduce the waiting time.
Immediate recommendations
It is also recommended to the MGH to use the same operating room for both the MD and RN in order to save the time and space. This will save the waiting time of the patient between pre-operative and post-operative care.
Action and Implementation plan
The above proposed suggestion can be carried out by instructing the patient's regarding entire plan followed by the appropriate rules. The legitimate rules should be created regarding the registered nurses. In addition, the MGH should teach the patient's regarding the electronic registrations and appointment standards and tell them that how could it reduce their waiting time. It is likewise important to educate the patient's regarding the appointment procedure that how the patient would able to take appointment with the booking App according to their choice of doctor and appropriate time frame. All of these initial steps are extremely important for the patients to know properly.
This would bring about decreased in waiting time, productive management activity and more prominent patient fulfillment. To oversee limit, the capacity of the enrolled medical caretaker should be expanded and the overall doctor ought to be accessible to treat patients with straightforward and viral contaminations or occasional illnesses......................
“Massachusetts General Hospital’s Pre-Admission Testing Area (Pata) Harvard Case” Solution
This is just a sample partial case solution. Please place the order on the website to order your own originally done case solution.